
Spine vascular malformation
- Home
- Spine vascular malformation
Spinal vascular malformation is a very rare condition. It is an abnormal tangle of blood vessels on, in, and/or near the spinal cord
Depending on where a malformation is located, it is classified as:an intramedullary arteriovenous malformation (AVM within the spinal cord tissue), a pial arteriovenous malformation (AVM on the surface), a dural spinal arteriovenous fistula (DAVF within the membrane that covers the spinal cord), or an epidural arteriovenous fistula (Epidural AVF on the surface of the membrane that covers the spinal cord).
Symptoms usually develop when people are in their 20s, although almost 20 percent of people diagnosed with spinal AVM are under the age of 16.
The emergence of symptoms may be sudden or gradual. Symptoms typically include:
As the condition progresses, additional symptoms may include:
The specific cause isn’t known. Most spinal AVMs are present at birth (congenital), but others may occur later in life.
Depending on the lesion, the best treatment plan changes. For intramedullary AVMs, partial or palliative treatment is sometimes an option since complete obliteration may carry a much higher chance of causing neurological deficits than conservative management or partial treatment.
The treatment strategy includes catheter embolization, surgical resection, radiation, and/or a combination these modalities.
For pial arteriovenous malformations, complete obliteration may be possible by surgical resection or catheter embolization depending on the anatomy.
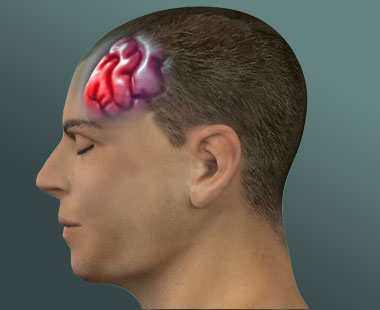
What is head injury?A traumatic brain injury, also referred to an acquired brain injury, occurs when someone suffers a sudden…
read more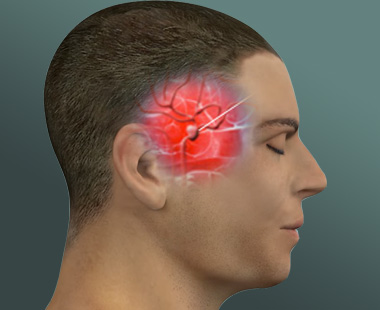
What is Brain Aneurysm?Brain aneurysm is an abnormal bulge in the brain's blood vessel. When it leaks or ruptures, it…
read more
What is a brain arteriovenous malformation ?Normally, arteries carry blood containing oxygen from the heart to the brain, and veins…
read more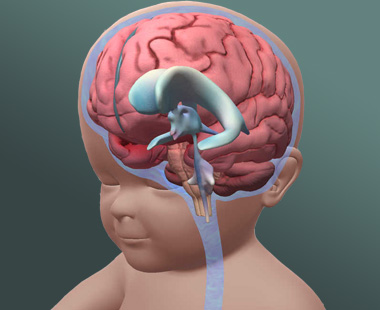
What is Hydrocephalus?Hydrocephalus is commonly referred to as "water on the brain." The so-called "water" is actually cerebrospinal fluid (CSF),…
read more